Abstract
Introduction:
Recent analyses have demonstrated that race and geographic area are important factors for outcomes in acute myeloid leukemia (AML) patients under the age of 60. Older patients with AML often receive outpatient therapy aimed at prolonging survival while maintaining time at home, a critical patient-centered outcome. We aimed to describe whether overall survival and time at home were associated with race, geographic area, and other baseline factors for older AML patients in the modern era of combination outpatient therapy including hypomethylating agents and Venetoclax.
Methods:
We identified all older adults (≥ 60 years) diagnosed with AML from 2015 - 2020 who received first-line treatment with Azacitidine (AZA), Azacitidine + Venetoclax (AZA+VEN), or other Venetoclax-containing regimens (Other VEN) within the University of North Carolina (UNC) Health System. Clinical and sociodemographic factors were captured.
The primary independent variables of interest were race, socioeconomic status (SES), rurality, and distance from UNC Cancer Center, an NCI Comprehensive Cancer Center (NCI-CCC). Race was self-reported. SES and rurality were estimated by ZIP code, as determined by Census tract information from the American Community Survey (2015-2019). Geocoding was used to estimate distance and travel time from patient's home address to the NCI-CCC.
The primary outcomes were overall survival (OS) and proportion of days engaged in oncologic services (PDEOS), which was defined as the proportion of person-days admitted, in the ED, at an office visit, or in infusion/transfusion divided by the overall number of person-days survived.
Linear and logistic regression analyses were performed to assess associations between independent variables and outcomes. Cox proportional hazards models were used to identify associations with OS. Multivariable analyses were performed using covariates of potential significance (p < 0.20).
Results:
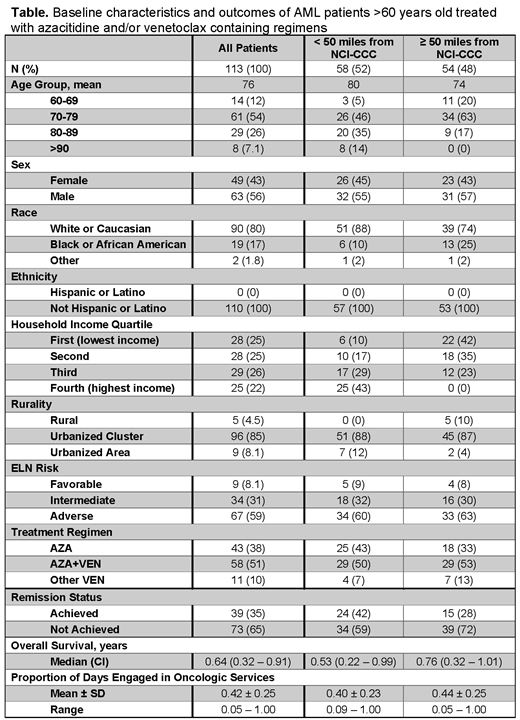
Of 136 newly diagnosed AML patients aged ≥ 60 years identified in the study period, 113 patients had full capture of service records (83%). These patients were treated with AZA (n = 43), AZA+VEN (n = 58), or other VEN (n = 11). Baseline demographics are shown in the Table. The median distance from the NCI-CCC was 42.3 miles. The median OS for the entire cohort was 0.64 years (CI 0.32 - 0.91). Mean PDEOS was 0.42. 35% of patients achieved remission (AZA = 14%, AZA+VEN = 52%; Other VEN = 27%).
Race, SES, and rurality were not significantly associated with survival, remission, PDEOS, or chemotherapy regimen received. Median OS was shorter for Black/AA patients (0.47 years, CI 0.23 - 1.25) than for White patients (0.64 years, CI 0.28 - 0.91), although this difference was not statistically significant (p = 0.80).
After adjusting for log years of follow-up time, distance from the NCI-CCC was associated with increased PDEOS. Patients who lived ≥ 50 miles from the NCI-CCC spent 7% more days engaged in oncologic services, which amounts to 2.1 more days per month (p = 0.03). No significant association was observed between distance from the NCI-CCC and OS. There was also no association seen between distance from the NCI-CCC and chemotherapy regimen received. We examined the association between PDEOS and age, ELN risk, and median household income, and none of these variables were significant enough in the model to be considered for multivariable analyses.
Conclusion:
Overall survival in this population of older AML patients was not significantly associated with race, SES, distance to NCI-CCC or rurality. Distance to treatment center was associated with increased burden of healthcare services. Patients who lived the greatest distances from the NCI-CCC spent a greater proportion of their days engaged in oncologic services. These conclusions are limited by the relative racial and ethnic homogeneity, lack of representation from urbanized and rural areas, and limited geographic location. Given the dismal median overall survival of only 7.7 months, targeted interventions including telehealth visits or consolidation of multidisciplinary care would likely be valuable for decreasing healthcare burden among older AML patients, especially for those with long distances to travel.
No relevant conflicts of interest to declare.